A newly characterized metabolite in urine could one day help predict whether tuberculosis treatment is working or not. Concentration of the glycopeptide, which researchers believe is a metabolite of a protein called plasma protease C1 inhibitor — increase significantly in the urine of people with active pulmonary tuberculosis. In people who respond to treatment, metabolite […]

A newly characterized metabolite in urine could one day help predict whether tuberculosis treatment is working or not. Concentration of the glycopeptide, which researchers believe is a metabolite of a protein called plasma protease C1 inhibitor — increase significantly in the urine of people with active pulmonary tuberculosis. In people who respond to treatment, metabolite levels dip back toward normal within a week. Though this initial study is small, such a test could help identify whether a candidate TB drug is likely to succeed or fail.
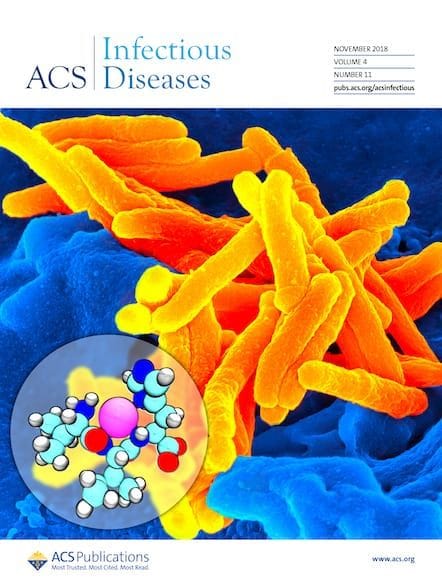
About a third of the world’s population — 1.8 billion people — is infected with Mycobacterium tuberculosis, the disease-causing bacterium, and new drugs to treat the disease are needed desperately. Current therapies fail in almost 1 out of 5 people, and treatment-resistant strains are becoming more prevalent. New drug trials are costly and challenging to run: researchers must treat patients for six months, and then follow up a year later to make sure the treatment worked, and the disease did not return.
“If you can identify patients early that have a higher likelihood to be cured by the treatment, then you may be able to reduce some complexity and the cost of the clinical trials,” says John Belisle, a microbiologist at Colorado State University. “The holy grail is if you can predict who’s going to relapse after the end of treatment.” That would provide a quick way to evaluate a drug’s efficacy early in the trial.
Several teams are looking for biomarkers that are affected by the disease. Belisle and his team decided to mine metabolites in urine — an easily-accessible biological fluid. In past work they identified several promising compounds whose levels changed during successful tuberculosis treatment. However, that study did not examine TB-infected people whose treatment failed.
Here, Belisle’s team used liquid chromatography with tandem mass spectrometry and enzymatic degradation to determine the structure of one of those metabolites, identifying it as a seryl-leucine core 1 O-glycosylated (SLC1G) peptide. They then measured it in the urine of 14 healthy individuals, 15 people with tuberculosis who were successfully treated with standard anti-TB treatment, 8 who failed treatment, and 12 in whom the treatment initially worked but the disease later recurred, at multiple points during the 6-month drug regimen.
In people whose treatment was successful, SLC1G levels fell approximately four-fold during the course of treatment, but did not drop significantly in people for whom the treatment ultimately didn’t work. Whether or not the therapy ultimately worked, higher SLC1G levels were associated with more lung inflammation and a higher bacterial load.
A biomarker like SLC1G “might allow faster evaluation of new drug regimens, for example, by showing early on whether patients are responding differentially to different novel regimens,” says Anna Upton, senior director of biology at TB Alliance, a nonprofit dedicated to developing better tuberculosis drugs. While the work is promising, she cautions, the small number of people in the study means that “further, larger studies are needed to see whether the associations seen here for SLC1G bear out in larger patient populations.”
The researchers are continuing their work with an expanded sample pool — and particularly with more people whose treatment ultimately failed. They are also developing a mass spectrometry assay that can more accurately quantify the peptide. If it holds up in further testing, Belisle believes SLC1G can be used as part of a molecular signature predicting treatment success.