Bile has a bad rap and often connotes an ill temper. But it plays a critical role in digestion and, thanks to new work, might eventually reduce the need for needles. While most people prefer oral medications to shots, many agents can’t be swallowed because gut enzymes would destroy molecules before they could work. To […]

Bile has a bad rap and often connotes an ill temper. But it plays a critical role in digestion and, thanks to new work, might eventually reduce the need for needles. While most people prefer oral medications to shots, many agents can’t be swallowed because gut enzymes would destroy molecules before they could work. To get around this problem, researchers have developed a possible strategy for delivering injectable medications orally. They coated nanoparticles with bile acids, which usher the payload through the intestinal cells and into the body.
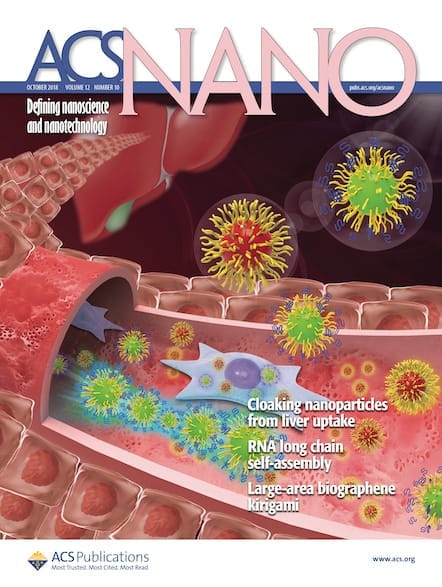
Getting macromolecules, such as proteins and DNA, into the bloodstream orally presents multiple hurdles. First, the agent must be shielded from the stomach’s hostile environment, which can be accomplished by stuffing the drug into a protective nanoparticle. But once the nanoparticles make it to the intestine, there’s another problem: Cells lining the intestine block nanoparticles’ absorption, and the tiny carriers simply pass out of the body unused. Chemically, nanoparticles, though, aren’t so different from globs of fat, which sail across the intestinal barrier with the help of bile acids, says You Han Bae of the University of Utah. “Fat is not water soluble, so it cannot be dissolved in the GI tract,” says Bae. “The bile acid is an emulsifier, a surfactant. It coats the fat like salad dressing, creating a nanoparticle of fat.” Receptors on the intestinal cells recognize bile acids and prompt cellular uptake. Bae wondered whether a drug-carrying nanoparticle coated in bile acids could be processed like those fats and cross the intestinal blockade.
In this proof of principle experiment, the researchers tested red fluorescent carboxylate polystyrene nanoparticles. “This plastic nanoparticle isn’t something we would ever actually use to deliver drugs in the body,” says Bae. “We were simply testing the bile acid strategy and figured we could find a biocompatible nanoparticle later if it worked.” The team chose glycocholic acid from the twelve naturally occurring bile acids because they could conjugate it to the nanoparticles using simple chemistry. It’s also relatively hydrophilic, which makes it less likely to self-aggregate, Bae says.
After treatment with bile-acid-coated nanoparticles, intestinal cells in culture began to glow red, indicating that they absorbed the nanoparticles. When the researchers fed the bile-acid-coated nanoparticles to rats, 47% of the particles crossed the intestinal wall, made their way into the lymphatic system, and then entered the bloodstream.
Going to the lymphatic system before entering the bloodstream may be a very good, though unexpected, finding, says Kathryn Whitehead of the Carnegie Mellon University who was not a part of the research. “If you want your drug to go to cells of the immune system, it is absolutely wonderful to get your particles into the lymphatic system where they live,” she says. “This gives us access to compartments in the body that we can’t usually access.” This route also bypasses the initial trip through the liver, she says. That step tends to reduce drug concentrations significantly.